These notes explain the following ideas related to signal detection theory.
There are two main components to the decision-making process: information aquisition and criterion.
Information acquisition: First, there is information in the CT scan. For example, healthy lungs have a characteristic shape. The presence of a tumor might distort that shape. Tumors may have different image characteristics: brighter or darker, different texture, etc. With proper training a doctor learns what kinds of things to look for, so with more practice/training they will be able to acquire more (and more reliable) information. Running another test (e.g., MRI) can also be used to acquire more information. Regardless, acquiring more information is good. The effect of information is to increase the likelihood of getting either a hit or a correct rejection, while reducing the likelihood of an outcome in the two error boxes.
Criterion: The second component of the decision process is quite different. For, in addition to relying on technology/testing to provide information, the medical profession allows doctors to use their own judgement. Different doctors may feel that the different types of errors are not equal. For example, a doctor may feel that missing an opportunity for early diagnosis may mean the difference between life and death. A false alarm, on the other hand, may result only in a routine biopsy operation. They may chose to err toward ``yes'' (tumor present) decisions. Other doctors, however, may feel that unnecessary surgeries (even routine ones) are very bad (expensive, stress, etc.). They may chose to be more conservative and say ``no'' (no turmor) more often. They will miss more tumors, but they will be doing their part to reduce unnecessary surgeries. And they may feel that a tumor, if there really is one, will be picked up at the next check-up.
These arguments are not about information Two doctors, with equally good training, looking at the same CT scan, will have the same information. But they may have a different bias/criteria.
External noise: There are many possible sources of external noise. There can be noise factors that are part of the photographic process, a smudge, or a bad spot on the film. Or something in the person's lung that is fine but just looks a bit like a tumor. All of these are to be examples of external noise. While the doctor makes every effort possible to reduce the external noise, there is little or nothing that they can do to reduce internal noise.
Internal noise: Internal noise refers to the fact that neural responses are noisy. To make this example really concrete, let's suppose that our doctor has a set of tumor detector neurons and that they monitor the response of one of these neurons to determine the likelihood that there is a tumor in the image (if we could find these neurons then perhaps we could publish and article entitled ``What the radiologist's eye tells the radiologist's brain''). These hypothetical tumor detectors will give noisy and variable responses. After one glance at a scan of a healthy lung, our hypothetical tumor detectors might fire 10 spikes per second. After a different glance at the same scan and under the same conditions, these neurons might fire 40 spikes per second.
Internal response: Now I do not really believe that there are tumor detector neurons in a radiologist's brain. But there is some internal state, reflected by neural activity somewhere in the brain, that determines the doctor's impression about whether or not a tumor is present. This is a fundamental issue; the state of your mind is reflected by neural activity somewhere in your brain. This neural activity might be concentrated in just a few neurons or it might be distributed across a large number of neurons. Since we do not know much about where/when this neural activity is, let's simply refer to it as the doctor's internal response.
This internal response is inherently noisy. Even when there is no tumor present (no-signal trials) there will be some internal response (sometimes more, sometimes less) in the doctor's sensory system.
Notice that we never lose the noise. The internal response for the signal-plus-noise case is generally greater but there is still a distribution (a spread) of possible responses. Notice also that the curves overlap, that is, the internal response for a noise-alone trial may exceed the internal response for a signal-plus-noise trial.
Figure 1: Internal response probability of occurrence curves for noise-alone and for signal-plus-noise trials.
Just to be really concrete, we could mark the horizontal axis in units of firing rate (10, 20, 30,..., etc. spikes per second). This would mean that on a noise-alone (no tumor) trial, it is most likely that the internal response would be 10 spikes per second. It is also rather likely that the internal response would be 5 or 15 spikes per second. But it is very unlikely that the internal response would be 25 spikes per second when no tumor is present. Because I want to remain noncommittal about what and where in the brain the internal response is, I did not label the horizontal axis in terms of firing rates. The internal response is in some unknown, but quantifiable, units.
The role of the criterion: Perhaps the simplest strategy that the doctor can adopt is to pick a criterion location along the internal response axis. Whenever the internal response is greater than this criterion they respond "yes''. Whenever the internal response is less than this criterion they respond "no''.
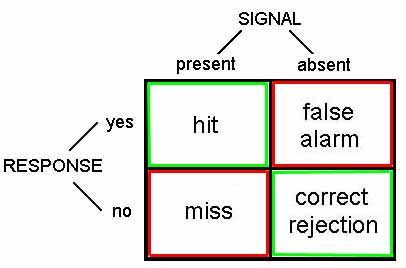
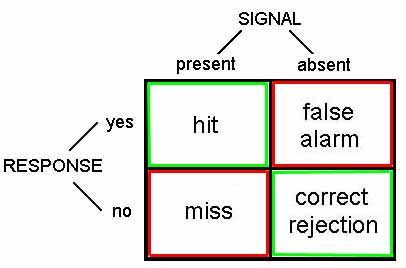
An example criterion is indicated by the vertical lines in Figure 2. The criterion line divides the graph into four sections that correspond to: hits, misses, false alarms, and correct rejections. On both hits and false alarms, the internal response is greater than the criterion, because the doctor is responding "yes''. Hits correspond to signal-plus-noise trials when the internal response is greater than criterion, as indicated in the figure. False alarms correspond to noise-alone trials when the internal response is greater than criterion, as indicated in the figure.
Figure 2: Internal response probability of occurrence curves for noise-alone and signal-plus-noise trials. Since the curves overlap, the internal response for a noise-alone trial may exceed the internal response for a signal-plus-noise trial. Vertical lines correspond to the criterion response.
Suppose that the doctor chooses a low criterion (Figure 3, top), so that they respond "yes'' to almost everything. Then they will never miss a tumor when it is present and they will therefore have a very high hit rate. On the other hand, saying "yes'' to almost everything will greatly increase the number of false alarms (potentially leading to unnecessary surgeries). Thus, there is a clear cost to increasing the number of hits, and that cost is paid in terms of false alarms. If the doctor chooses a high criterion (Figure 3, bottom) then they respond "no'' to almost everything. They will rarely make a false alarm, but they will also miss many real tumors.
Figure 3: Effect of shifting the criterion
Notice that there is no way that the doctor can set their criterion to achieve only hits and no false alarms. The message that you should be taking home from this is that it is inevitable that some mistakes will be made. Because of the noise it is simply a true, undeniable, fact that the internal responses on noise-alone trials may exceed the internal responses on signal-plus-noise trials, in some instances. Thus the doctor cannot always be right. They can adjust the kind of errors that they make by manipulating their criterion, the one part of this diagram that is under their control.
ROC curves (Figure 4) are plotted with the false alarm rate on the horizontal axis and the hit rate on the vertical axis. We already know that if the criterion is high, then both the false alarm rate and the hit rate will be very low. If we move the criterion lower, then the hit rate and the false alarm rate both increase. So the full ROC curve has an upward sloping shape. Notice also that for any reasonable choice of criterion, the hit rate is always larger than the false alarm rate, so the ROC curve is bowed upward. The ROC curve characterizes the choices available to the doctor. They may set the criterion anywhere, but any choice that they make will land them with a hit and false alarm rate somewhere on the ROC curve.
Figure 4: Internal response probability of occurrence curves and ROC curves for different signal strengths. When the signal is stronger there is less overlap in the probability of occurrence curves, and the ROC curve becomes more bowed.
The role of information: Aquiring more information makes the decision easier. Running another test (e.g., MRI) can be used to acquire more information about the presence or absence of a tumor. Unfortunately, the radiologist does not have much control over how much information is available.
In a controlled perception experiment the experimenter has complete control over how much information is provided. Having this control allows for quite a different sort of outcome. If the experimenter chooses to present a stronger stimulus, then the subject's internal response strength will, on the average, be stronger. Pictorially, this will have the effect of shifting the probability of occurrence curve for signal-plus-noise trials to the right, a bit further away from the noise-alone probability of occurrence curve.
Figure 4 shows two sets of probability of occurrence curves and two ROC curves. When the signal is stronger there is less overlap between the two probability of occurrence curves. When this happens the subject's choices are not so difficult as before. They can pick a criterion to get nearly a perfect hit rate with almost no false alarms. ROC curves for stronger signals bow out further than ROC curves for weaker signals.
Varying the noise: For stronger signals, the probability of occurrence curve for signal-plus-noise shifts right and detection is easier. There is another aspect of the probability of occurrence curves that also determines detectability: the spread of the curves. For example, consider the two probability of occurrence curves in Figure 5. The separation between the peaks is the same but the second set of curves are much skinnier. Clearly, the signal is much more discriminable when there is less spread (less noise) in the probability of occurrence curves. So the subject would have an easier time setting their criterion in order to be right nearly all the time.
Figure 5: Internal response probability of occurrence curves for two different noise levels. When the noise is greater, the curves are wider (more spread) and there is more overlap.
Discriminability index (d'): Thus, the discriminability of a signal depends both on the separation and the spread of the noise-alone and signal-plus-noise curves. To write down a complete description of how discriminable the signal is from no-signal, we want a formula that captures both the separation and the spread. The most widely used measure is called d-prime (d' ), and its formula is simply:
d' = separation / spread
This number, d', is an estimate of the strength of the signal. Its primary virtue, and the reason that it is so widely used, is that its value does not depend upon the criterion the subject is adopting, but instead it is a true measure of the internal response.
Estimating d': To recap... Increasing the stimulus strength separates the two (noise-alone versus signal-plus-noise) probability of occurrence curves. This has the effect of increasing the hit and correct rejection rates. Shifting to a high criterion leads to fewer false alarms, fewer hits, and fewer surgical procedures. Shifting to a low criterion leads to more hits (lots of worthwhile surgeries), but many false alarms (unnecessary surgeries) as well. The discriminability index, d', is a measure of the strength of the internal response that is independent of the criterion.
But how do we measure d'? The trick is that we have to measure both the hit rate and the false alarm rate, then we can read-off d' from an ROC curve. Figure 4 shows a family of ROC curves. Each of these curves corresponds to a different d-prime value; d'=0, d'=1, etc. As the signal strength increases, the internal response increases, the ROC curve bows out more, and d' increases.
So let's say that we do a detection experiment; we ask our doctor to detect tumors in 1000 CT scans. Some of these patients truly had tumors and some of them didn't. We only use patients who have already had surgery (biopsies) so we know which of them truly had tumors. We count up the number of hits and false alarms. And that drops us somewhere on this plot, on one of the ROC curves. Then we simply read off the d' value corresponding to that ROC curve. Notice that we need to know both the hit rate and the false alarm rate to get the discriminability index, d'.
Medical Malpractice Example: A study of doctors' performance was performed in Boston. 10,000 cases were analyzed by a special commission. The commission decided which were handled negligently and which well. They found that 100 were handled very badly and there is good cause for a malpractice suit. Of these 100, only 20 cases were pursued. What should we conclude?
Ralph Nader and others concluded that doctors are not being sued enough. But this conclusion was based on only partial information (hits and misses). I did not tell you what happened in the other 9900 cases. How many law suits were there in those cases? What if there were many (e.g., 9000 out of 9900) false alarms? The AMA concluded that doctors are being sued too much.